Serious and deadly small vessel vasculitis with multi-organ involvement due to COVID mRNA vaccination e.g. Pfizer; we are seeing cases of small & large vessel vaccine-induced vasculitis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9118190/
The case of a 77-year-old woman who developed small-vessel vasculitis with multiorgan involvement after receiving the BNT162b2 COVID-19 vaccine (Pfizer and BioNTech, New York City, NY, USA).
The case:
‘A 77-year-old woman visited the emergency room because of weakness and weight loss persisting for 1 month. She had received the second dose of the Pfizer-BioNTech COVID-19 vaccine 1 month previously, following which she experienced fever and myalgia. The symptoms persisted and were accompanied by anorexia, sweating, and weight loss. Furthermore, she presented with dyspnea, dizziness, and an ear fullness sensation. She had no specific medical history except for hypertension, and no other new drug history. Her vital signs were stable: blood pressure 120/80 mm Hg; pulse rate 71 beats/min; respiratory rate 21 breaths/min; and temperature 36.5 °C. Physical examination revealed hyperemia in both eyes and livedo reticularis of the upper and lower extremities; however, joint swelling or tenderness was not observed. Blood test results revealed a white blood cell count of 15,000/µL and markedly elevated high-sensitivity C‑reactive protein levels at 38 mg/dL. Furthermore, she had azotemia accompanied by high creatinine levels (6 mg/dL); urinalysis showed 200 erythrocytes/µL (3+) and 15 leukocytes/µL. The spot urine protein-to-creatinine ratio was 4700 mg/g Cr, showing nephrotic-range proteinuria.
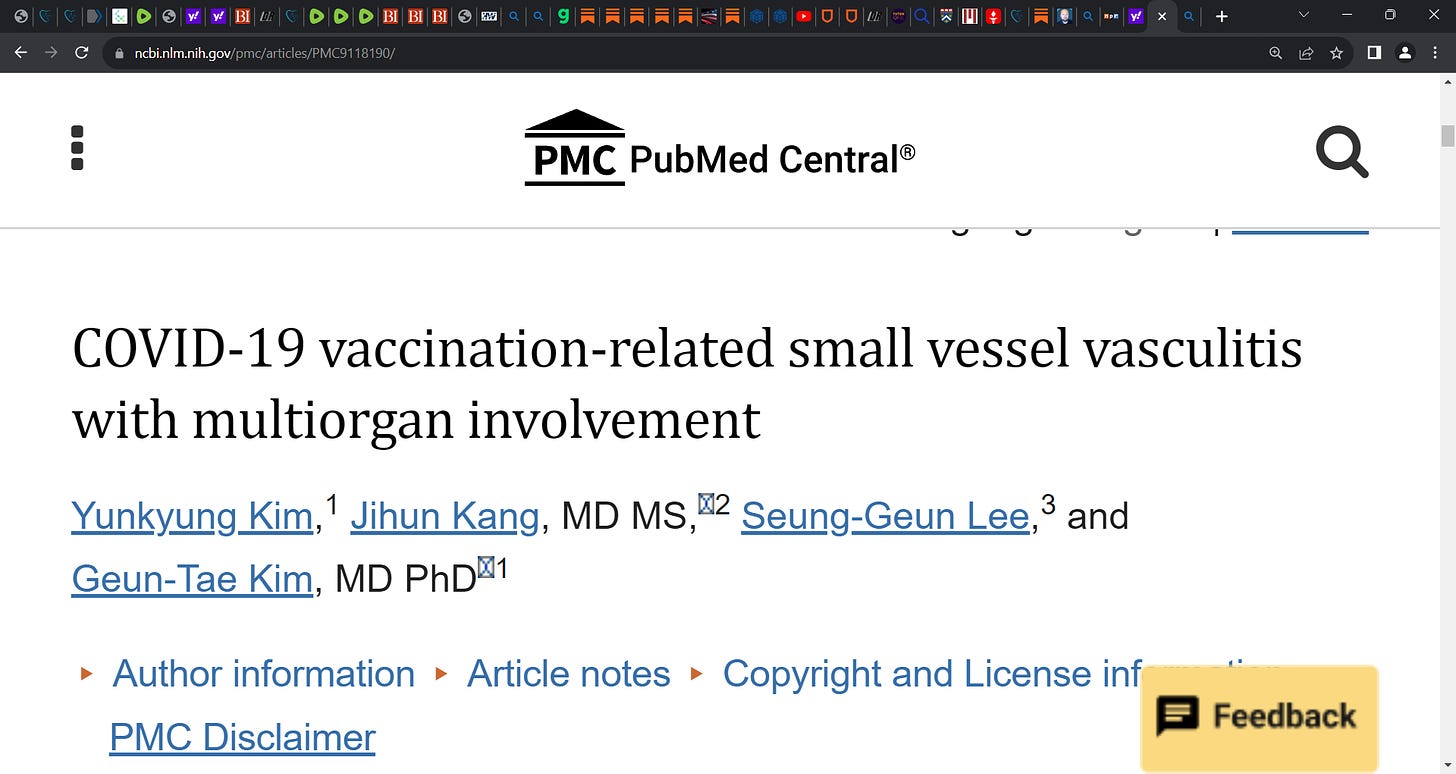
Regarding hyperemia in both eyes, slit-lamp examination was performed, showing conjunctivitis. Tympanometry was performed for the ear fullness sensation, and bilateral otitis media with effusion was confirmed (Fig. 1a).
a tympanogram of the left ear with effusion of tympanic membranes; b computed tomography (CT) image of the chest showing variable sized enhancing nodules in both lungs, with lower lung zone predominance; c positron-emission tomography/CT image
Chest computed tomography (CT) imaging revealed enhancing nodules of variable sizes in bilateral lungs; the nodules were predominantly observed in the lower lung zone, suggesting atypical pneumonia or pulmonary metastasis (Fig. 1b). Empirical antibiotic therapy was initiated for managing pneumonia. Positron-emission tomography/CT was performed for the differential diagnosis of the pulmonary lesions; the findings showed inflammatory changes suggestive of vasculitis rather than metastasis (Fig. 1c).
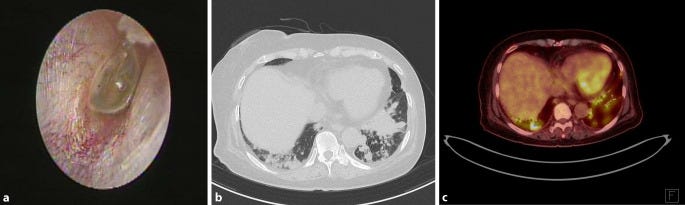
Serologic test results revealed an elevated antinuclear antibody titer (1:320), moderate anticentromere antibody titer, and low rheumatoid factor titer; renal biopsy was performed to determine the cause of severe proteinuria. Crescentic glomerulonephritis was observed using light microscopy (Fig. 2a, b); no immune complexes were observed using immunofluorescence and electron microscopy (Fig. 2c).
a Light microscopy of the glomerulus (periodic acid-Schiff, × 200); b Masson trichrome stain, × 200; c electron microscopy, × 2000
Small-vessel vasculitis was diagnosed on the basis of systemic symptoms (weight loss and fever), conjunctivitis, otitis media, livedo reticularis, lung nodules leading to the suspicion of vasculitis, and pauci-immune glomerulonephritis.
Methylprednisolone (1 mg/kg and day) was initiated for vasculitis management. Hemodialysis was performed to correct azotemia and acidosis. The patient exhibited gradual improvement in general and respiratory symptoms. One month after starting the treatment, follow-up chest CT imaging revealed markedly decreased nodules; furthermore, the inflammatory marker levels had recovered to normal. However, the patient had to undergo permanent dialysis owing to several irreversible glomerular sclerotic changes. During steroid dose tapering, she was started on azathioprine. She remains well without recurrence.’



A young family member was diagnosed with Behçet’s disease last year. The docs blamed it on recessive genes 🙄. No mention that the jabs she took for college might be the cause
Does "and/or" mean that all 15 vasculitis patients referred to below got the clot shots?
"Here we describe a cohort of 15 patients with vasculitis temporally associated with COVID-19 disease and/or COVID-19 vaccine."
"In conjunction with the novel SARS-CoV-2 virus, over 70 different, more or less severe, systemic and/or organ-specific immune-mediated complications have been reported, vasculitis being one of them.1"
Vasculitis as Temporally Associated With COVID-19 Infection or Vaccination: A Single-center Experience
https://www.jrheum.org/content/49/2/232