"Antibody-dependent enhancement (ADE) and SARS-CoV-2 vaccines and therapies"; "ADE is a concern" for those who have been vaccinated for Covid-19 (Lee et al., NATURE).
Previous respiratory syncytial virus and dengue virus vaccine studies revealed human clinical safety risks related to ADE, resulting in failed vaccine trials.
‘Data from the study of SARS-CoV and other respiratory viruses suggest that anti-SARS-CoV-2 antibodies could exacerbate COVID-19 through antibody-dependent enhancement (ADE).’
SOURCE:
Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies
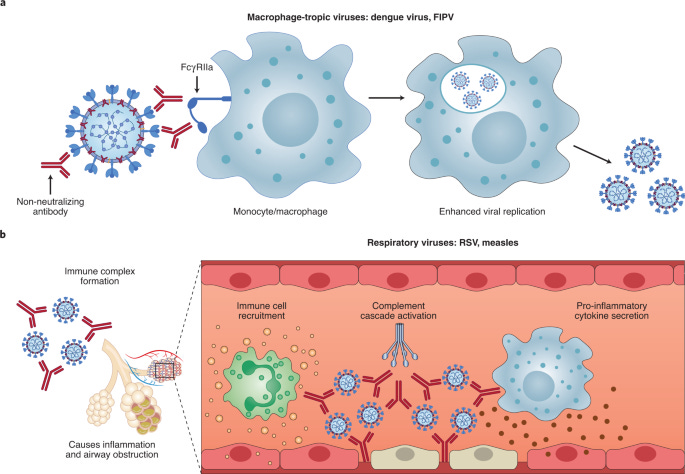
‘One potential hurdle for antibody-based vaccines and therapeutics is the risk of exacerbating COVID-19 severity via antibody-dependent enhancement (ADE). ADE can increase the severity of multiple viral infections, including other respiratory viruses such as respiratory syncytial virus (RSV)9,10 and measles11,12.’
‘Scientists say that with ADE, after people get vaccinated for an initial virus, infection by a subsequent variant or strain of the virus can result in "increased viral replication and more severe disease, leading to major safety risks."
"Non-neutralizing antibodies generated by past infection or vaccination fail to shut down the pathogen upon re-exposure. Instead, they act as a gateway by allowing the virus to gain entry and replicate in cells that are usually off limits... That, in turn, can lead to wider dissemination of illness, and over-reactive immune responses that cause more severe illness," according to scientists.’
What is ADE?
ADE occurs when the antibodies generated during an immune response recognize and bind to a pathogen, but they are unable to prevent infection. Instead, these antibodies act as a “Trojan horse,” allowing the pathogen to get into cells and exacerbate the immune response.
Is ADE caused by vaccines?
On a few occasions ADE has resulted from vaccination:
Respiratory syncytial virus (RSV) — RSV is a virus that commonly causes pneumonia in children. A vaccine was made by growing RSV, purifying it, and inactivating it with the chemical formaldehyde. In clinical trials, children who were given the vaccine were more likely to develop or die from pneumonia after infection with RSV. As a result of this finding, the vaccine trials stopped, and the vaccine was never submitted for approval or released to the public.
Measles — An early version of measles vaccine was made by inactivating measles virus using formaldehyde. Children who were vaccinated and later became infected with measles in the community developed high fevers, unusual rash, and an atypical form of pneumonia. Upon seeing these results, the vaccine was withdrawn from use, and those who received this version of the vaccine were recommended to be vaccinated again using the live, weakened measles vaccine, which does not cause ADE and is still in use today.
A more recent example of ADE following vaccination comes from dengue virus:
Dengue virus — In 2016, a dengue virus vaccine was designed to protect against all four serotypes of the virus. The hope was that by inducing immune responses to all four serotypes at once, the vaccine could circumvent the issues related to ADE following disease with dengue virus. The vaccine was given to 800,000 children in the Philippines. Fourteen vaccinated children died after encountering dengue virus in the community. It is hypothesized that the children developed antibody responses that were not capable of neutralizing the natural virus circulating in the community. As such, the vaccine was recommended only for children greater than 9 years of age who had already been exposed to the virus.
Risk of ADE for SARS-CoV-2 vaccines
‘Evidence for vaccine-induced ADE in animal models of SARS-CoV is conflicting, and raises potential safety concerns. Liu et al. found that while macaques immunized with a modified vaccinia Ankara viral vector expressing the SARS-CoV S protein had reduced viral replication after challenge, anti-S IgG also enhanced pulmonary infiltration of inflammatory macrophages and resulted in more severe lung injury compared to unvaccinated animals66. They further showed that the presence of anti-S IgG prior to viral clearance skewed the wound-healing response of macrophages into a pro-inflammatory response. In another study, Wang et al. immunized macaques with four B-cell peptide epitopes of the SARS-CoV S protein and demonstrated that while three peptides elicited antibodies that protected macaques from viral challenge, one of the peptide vaccines induced antibodies that enhanced infection in vitro and resulted in more severe lung pathology in vivo67.
In contrast, to determine whether low titres of neutralizing antibodies could enhance infection in vivo, Luo et al. challenged rhesus macaques with SARS-CoV nine weeks post-immunization with an inactivated vaccine, when neutralizing antibody titres had waned below protective levels68. While most immunized macaques became infected following viral challenge, they had lower viral titres compared to placebo controls and did not show higher levels of lung pathology. Similarly, Qin et al. showed that an inactivated SARS-CoV vaccine protected cynomolgus macaques from viral challenge and did not result in enhanced lung immunopathology, even in macaques with low neutralizing antibody titres69. A study in hamsters demonstrated that despite enhanced in vitro viral entry into B cells via FcγRII, animals vaccinated with the recombinant SARS-CoV S protein were protected and did not show enhanced lung pathology following viral challenge70.
SARS-CoV immunization studies in animal models have thus produced results that vary greatly in terms of protective efficacy, immunopathology and potential ADE, depending on the vaccine strategy employed. Despite this, vaccines that elicit neutralizing antibodies against the S protein reliably protect animals from SARS-CoV challenge without evidence of enhancement of infection or disease71,72,73. These data suggest that human immunization strategies for SARS-CoV-2 that elicit high neutralizing antibody titres have a high chance of success with minimal risk of ADE. For example, subunit vaccines that can elicit S-specific neutralizing antibodies should present lower ADE risks (especially against S stabilized in the prefusion conformation, to reduce the presentation of non-neutralizing epitopes8). These modern immunogen design approaches should reduce potential immunopathology associated with non-neutralizing antibodies.
Vaccines with a high theoretical risk of inducing pathologic ADE or ERD include inactivated viral vaccines, which may contain non-neutralizing antigen targets and/or the S protein in non-neutralizing conformations, providing a multitude of non-protective targets for antibodies that could drive additional inflammation via the well-described mechanisms observed for other respiratory pathogens. However, it is encouraging that a recent assessment of an inactivated SARS-CoV-2 vaccine elicited strong neutralizing antibodies in mice, rats and rhesus macaques, and provided dose-dependent protection without evidence of enhanced pathology in rhesus macaques74. Going forward, increased vaccine studies in the Syrian hamster model may provide critical preclinical data, as the Syrian hamster appears to replicate human COVID-19 immunopathology more closely than rhesus macaque models75.’



Kennedy called this out at the beginning. We see this on the elderly that get vaccinated and especially with flu shots (another reason they're worthless). Aside from stroke or MI, it's a good bet that ADE killed many seniors through infection enhancement.
All the i believe ferrets upon rechallenge with a variant died from ade. All of them. I knew that in 2020 and I was like the vaccine failed in animal trials. Why are they going forward.....