
Appelbaum et al.: "SARS-CoV-2 spike-dependent platelet activation in COVID-19 vaccine-induced thrombocytopenia"
'Our serologic investigations highlight a potential mechanism for COVID-19 VIT involving SARS-CoV-2 spike-dependent FcγRIIa-mediated platelet activation.'
SOURCE:
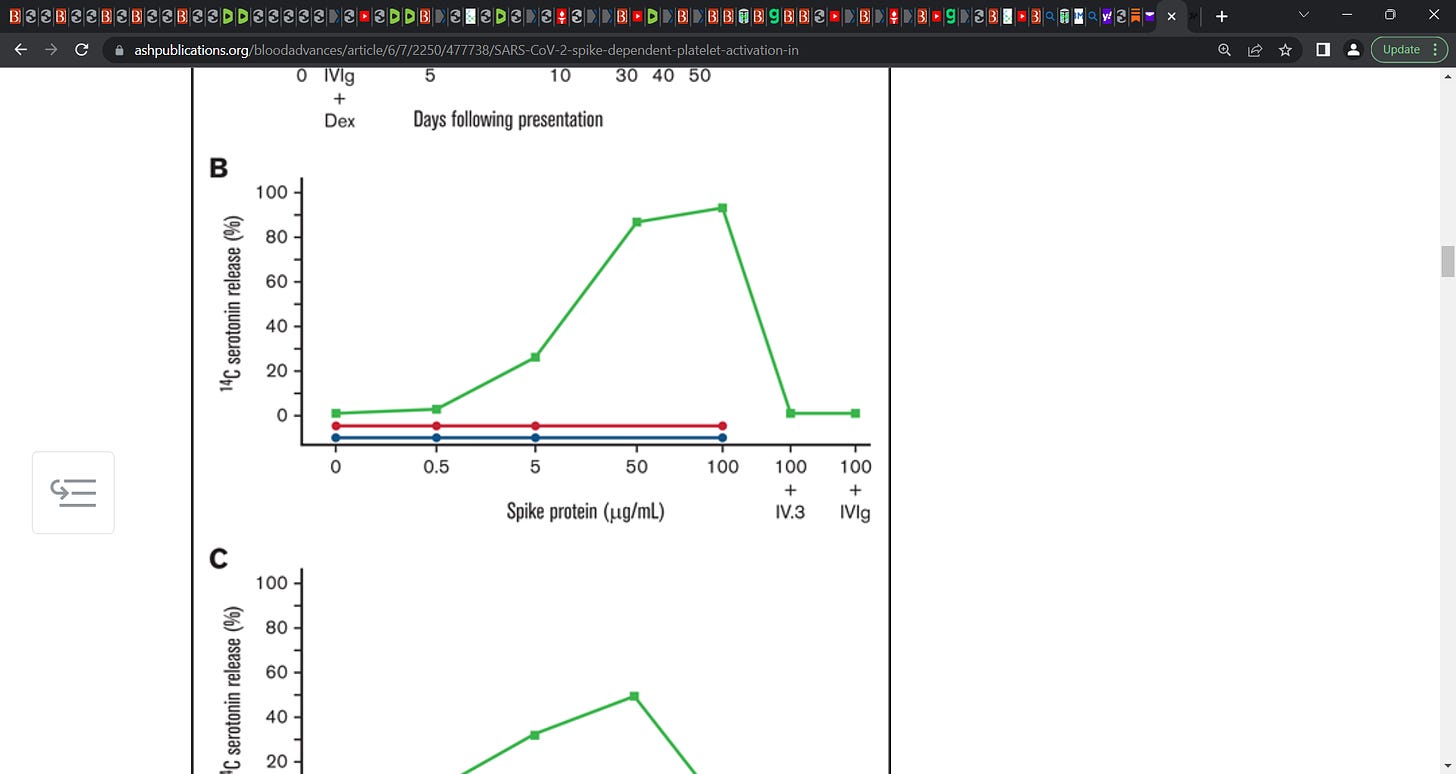
“Our patient was a 25-year-old woman who presented to the hospital 10 days after receiving the Moderna mRNA COVID-19 vaccine with fatigue, petechiae, and wet purpura. The initial platelet count was 1 × 109/L 1000/mm3 without evidence of schistocytes on blood smear (Figure 1A). Coagulation studies were within the normal range, including prothrombin time of 13.6 seconds (normal, 10.7-15.6 seconds), international normalized ratio of 1.1 (normal, 0.8-1.3), and partial thromboplastin time of 30 seconds (normal, 22-35 seconds). The presence of a lupus anticoagulant was likely excluded, given the use of a lupus-sensitive reagent for partial thromboplastin time testing. Anti-PF4/heparin antibodies were not detected (optical density [OD], 0.221) and the SRA tests, with or without heparin or exogenous PF4, were negative. Assays for drug-induced immune thrombocytopenia with washed donor platelets as above were also negative for platelet binding with vaccine, PEG2000, or SARS-CoV-2 spike protein.
Our serologic investigations highlight a potential mechanism for COVID-19 VIT involving SARS-CoV-2 spike-dependent FcγRIIa-mediated platelet activation. Similar immune complex–mediated platelet activation has also been observed with severe COVID-19 infection.2,4 The mechanism described here resembles platelet activation seen in HIT but does not involve anti-PF4/heparin antibodies. HIT serves as a useful analogy, but certain key differences were noted in our patient. Notably, our patient presented with bleeding symptoms as opposed to thrombosis; however, in parallel to HIT, not all patients with platelet-activating antibodies develop thrombosis.10
Finally, it is unclear why only a minority of patients with anti-spike antibodies exhibit thrombocytopenia and platelet activation. One hypothesis is that platelet activation is dependent on unique spike protein epitopes, which are recognized by only a minority of identified antibodies, as seen in HIT.11 Therefore, using our knowledge of platelet activation from studying HIT, we propose this mechanism for COVID-19 VIT involving SARS-CoV-2 anti-spike antibodies.’












It's amazing. I have at least four highly waxed friends who are totall Believers in the mainstream narrative who have gotten clots in various places soon after there injections. Pulmonary embolism, stroke etc. Yet they refuse to even hear that there might be a connection. I don't understand any of this. One of them had just gotten a booster and came down with pulmonary embolism. She and the doctor are blaming it on a case of covid she had last summer, instead of the booster she had this month. Mind-blowing
It is good to start finally getting possible mechanisms figured out. We need this badly.