
Fulminant 'severe; myocarditis ending in death following mRNA technology based COVID vaccination; an autopsy case of a 27-year-old healthy man who presented with cardiopulmonary arrest 8 days after
the first dose of the Moderna mRNA SARS-CoV-2 vaccine and was finally diagnosed with fulminant myocarditis and he died; microscopic findings revealed that significant mixed inflammatory infiltration
SOURCE:
https://www.sciencedirect.com/science/article/pii/S1878540922001128
‘A 27-year-old man was transferred to the emergency room in cardiopulmonary arrest. The patient had just received the first dose of the mRNA-1273 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine (Moderna, Cambridge, MA, USA) 8 days earlier and had no symptoms such as chest pain suspected of myocarditis or general fatigue suspected of low cardiac output after the vaccination until the emergency room visit. He had a high exercise habit; his teammates called for an ambulance when he was found sitting unconscious during practice. Upon arrival at the emergency room, he presented asystole. Despite cardiopulmonary resuscitation, fatal ventricular arrhythmias (Fig. 1A) repeated, and he eventually received venoarterial extracorporeal membrane oxygenation (VA-ECMO) and Impella CP (Abiomed, Danvers, MA, USA), after 2 h of his visit. A chest radiograph obtained in an emergency room showed an enlarged heart and pulmonary congestion (Fig. 1E). The patient had undergone orthopedic surgery 3 months before the recent hospitalization. An electrocardiogram (ECG) abnormality and mild cardiac shadow enlargement in chest radiograph had been noted preoperatively (Fig. 1B, D); however, since he was asymptomatic, no further examination was performed. Additionally, he had no family history of cardiovascular disease or sudden death.
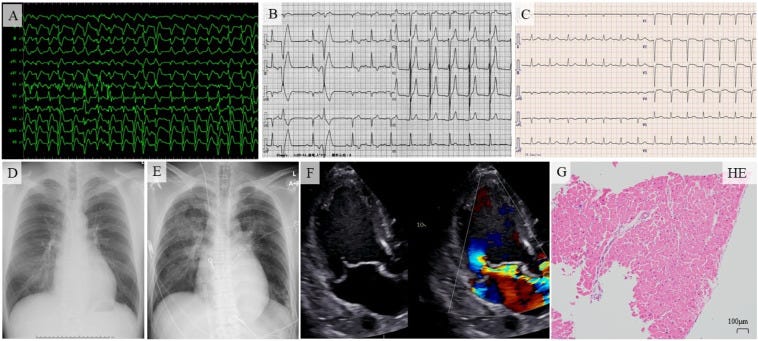
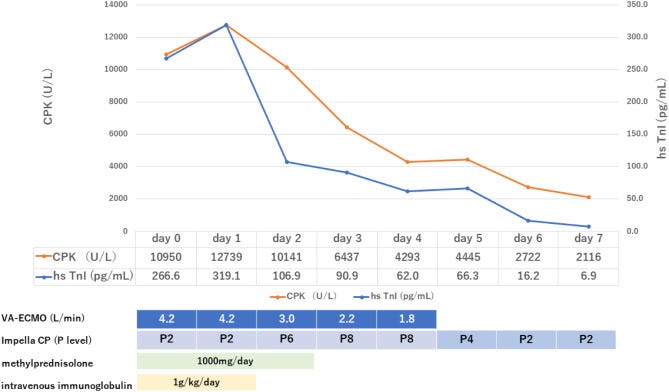
On admission to the coronary care unit, blood pressure was 81/45 mmHg, pulse rate was 73/min, and the temperature was 37.2 °C with VA-ECMO at 2.2 L/min, noradrenaline at 0.4 μg/kg/min, and dobutamine at 1.0 μg/kg/min. The nasopharyngeal SARS-CoV-2 polymerase chain reaction test was negative. ECG showed sinus rhythm, right-axis deviation, and poor R-wave progression (Fig. 1C). Blood tests revealed severe liver and kidney dysfunction, lactic acidosis, elevated highly sensitive troponin I level, with no significant increase in eosinophil count. Transthoracic echocardiography showed that left ventricular end-diastolic diameter increased to 77 mm and left ventricular ejection fraction (LVEF) decreased to 25 %. Right ventricular contraction also decreased severely. The left ventricular wall thickness was 14 mm, slightly thickened, and there was a small amount of pericardial effusion. Furthermore, the posterior leaflet of the mitral valve was significantly prolapsed, which indicated severe mitral regurgitation (MR) (Fig. 1F). There was no evidence of vegetation or ruptured chordae tendineae. Coronary angiography showed normal coronary arteries, and we performed endomyocardial biopsy from the right ventricular side of ventricular septum and obtained three specimens. We considered the patient to have fulminant myocarditis developed in the presence of stage B heart failure due to chronic severe MR and started corticosteroid pulse therapy (methylprednisolone 1000 mg/day for 3 days) and intravenous immunoglobulin (IVIG) therapy (1 g/kg for 2 days). The results of the endomyocardial biopsy were no inflammatory findings in the myocardium in all three specimens (Fig. 1G). After initiation of ventricular assist devices with VA-ECMO and Impella CP, steroid pulse therapy, and IVIG therapy, cardiac enzyme level decreased (Fig. 2). He was able to wean off VA-ECMO on day 4; however, anisocoria appeared on the same day and head computed tomography revealed diffuse severe brain edema. On day 7, his LVEF improved to 45 %, and Impella CP was weaned. On day 9, the electroencephalogram became flat. The patient died on day 28 due to progressive multiorgan failure. The blood eosinophil count showed no significant increase until his death.
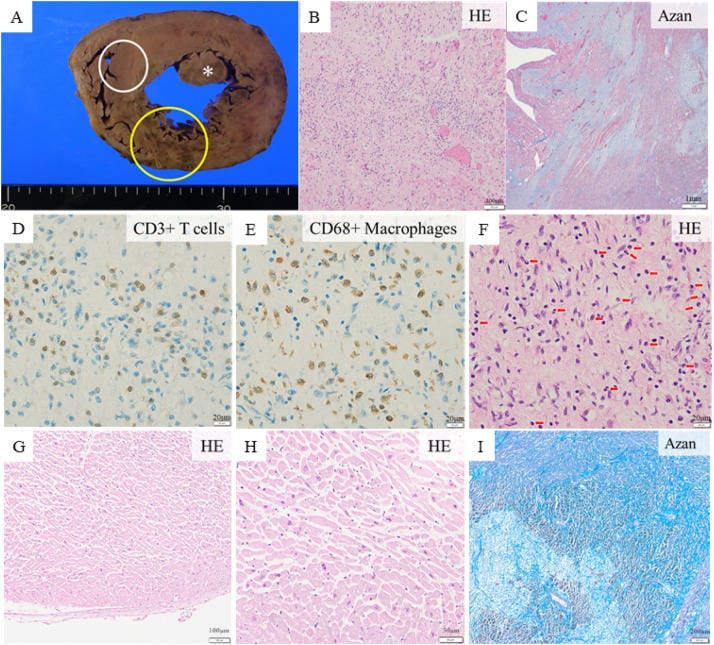
An autopsy revealed asymmetric left ventricular hypertrophy, thickening of the right ventricular wall (550 g; LV wall, 11–16 mm; RV wall, 5–7 mm), myxomatous degeneration of the posterior leaflet of the mitral valve, and hypertrophy of the posteromedial papillary muscle (Fig. 3A). Microscopic findings revealed that cardiac myocytolysis and widespread fibrosis were observed (Fig. 3B, C) and significant mixed inflammatory infiltration (T cells, macrophages, and eosinophils) was observed in the left ventricular free wall and the anterior potion of the ventricular septum (Fig. 3D–F), which led to the diagnosis of myocarditis. There was no evidence of CD138+ CD79a+ CD20− plasmocytes. Although asymmetric left ventricular hypertrophy was observed, cardiac muscle cell disorganization that is characteristic of hypertrophic cardiomyopathy was not observed. In contrast to the left ventricular free wall, the posterior potion of the ventricular septum and right ventricular free wall had almost no inflammatory cell infiltration or fibrosis, and almost normal myocardium was maintained (Fig. 3G, H). Additionally, the posterior papillary muscles showed a similar inflammatory cell infiltrate at the left ventricular myocardium, with extensive and severe fibrosis (Fig. 3I).
Discussion
We report an autopsy case of a 27-year-old healthy man who presented with cardiopulmonary arrest 8 days after the first dose of the mRNA-1273 SARS-CoV-2 vaccine and was finally diagnosed with fulminant myocarditis. Mitral valve prolapse is relatively common in athletes, also known as arrhythmic mitral valve prolapse, and may present with ventricular arrhythmias and sudden cardiac death even in the absence of hemodynamic impairment [[4], [5], [6]]. In this case, endomyocardial biopsy performed before death showed no evidence of myocarditis; therefore, cardiopulmonary arrest due to arrhythmic mitral valve prolapse was considered a possible differential diagnosis. However, the autopsy showed obvious severe myocardial inflammation findings, leading to the diagnosis of myocarditis. It is difficult to distinguish hypertrophic cardiomyopathy from the athlete's heart occasionally [7], the patient presented with asymmetric left ventricular hypertrophy, but no findings characteristic of hypertrophic cardiomyopathy were seen on autopsy. Therefore, we considered that his left ventricular hypertrophy was a consequence of the athlete's heart and MR. Microscopic findings showed infiltration of T cells, macrophages, and eosinophils. Such myocarditis with lymphocytic and eosinophilic infiltration has been reported after mRNA COVID-19 vaccination [3,8]. Lymphocytic and eosinophilic infiltration was also observed in myocarditis after smallpox vaccination and a mechanism of immune-mediated myocarditis has been speculated [9]. In addition, Frustaci et al. reported three cases of pathohistologically defined eosinophilic myocarditis after COVID19 vaccination, referring to the possibility of eosinophilic myocarditis (hypersensitivity myocarditis) as an allergic reaction and the possibility that immunosuppressive therapy including steroids may be effective [10]. Considering the response to steroid pulse therapy, it is possible that this mechanism of eosinophil-mediated immunological injury to cardiomyocytes is also involved in this case. This patient's eosinophilic infiltrate may have decreased from the time of onset because of the 4-week interval between onset and death and steroid treatment. Microscopic findings of the posterior potion of the ventricular septum showed no inflammatory cell infiltrate, and the myocardial biopsy findings are consistent with a sampling error. If the endomyocardial biopsy results were not a sampling error, then his first fatal arrhythmia was caused by arrhythmic mitral valve prolapse and athlete's heart, with myocarditis occurring afterward. However, considering his sequence of events integrally, it is still highly likely that it was a sampling error. Fibrosis of the papillary muscle and myocardium is also observed in patients with arrhythmic mitral valve prolapse, and similar findings were noted in this case [5,6]. This may indicate that the patient had an arrhythmogenic substrate and was more susceptible to fatal arrhythmias.
Conclusions
Here, we reported an autopsy case of fulminant myocarditis following mRNA COVID-19 vaccination. The microscopic findings revealed that significant mixed inflammatory infiltration (T cells, macrophages, and eosinophils) and widespread fibrosis were observed in the left ventricle. Steroid therapy may be effective in the treatment of fulminant myocarditis following mRNA COVID-19 vaccination.’










These monsters have talked themselves into believing they're saving the world. Covid scientism is the new worldwide religion.
There's a new church in town. Watch CHURCH OF THE PANDEMIC MIND. https://turfseer.substack.com/p/church-of-the-pandemic-mind
Dr. Shankara Chetty the doctor who treat over 10,000 Covid patients and no death or ventilation in South Africa, said on the eighth day after catching Covid you get worst symptoms always on the eighth day. If catch earlier,Dr Chetty use mostly antihistamines and steroids to treat Covid patients. Dr. Chetty said people are dying not from virus but from allergic reactions to spike proteins.