
Did recent Buhre et al. FRONTIERS publication add to Irrgang et al. Science Immunology finding of potential immune tolerance (IgG4 class switch) among anti-S vaccinal Ab responses with repeat doses?
It appears that the IgG4 class switch & tolerance is due to the mRNA platform & with repeated doses & principally more so via Moderna shots that generate detectable long-term IgG4 responses
What is out concern? The concern is that with potential class switching (due to repeat COVID injections/boosters) towards the IgG4 class (a non-inflammatory Ab), this can promote immune tolerance and as such a sub-optimal immune response. That is the key question in that has the COVID gene injection driven immune tolerance or some amount of it that can be problematic to the vaccinee (s)? Is this pathological? We need additional research (urgent) yet the 2 studies by Buhre and Irrgang presented here points to an unusual circumstance of increasing tolerance especially with repeated dosing of this COVID gene injection.
Buhre et al.:
SOURCE:
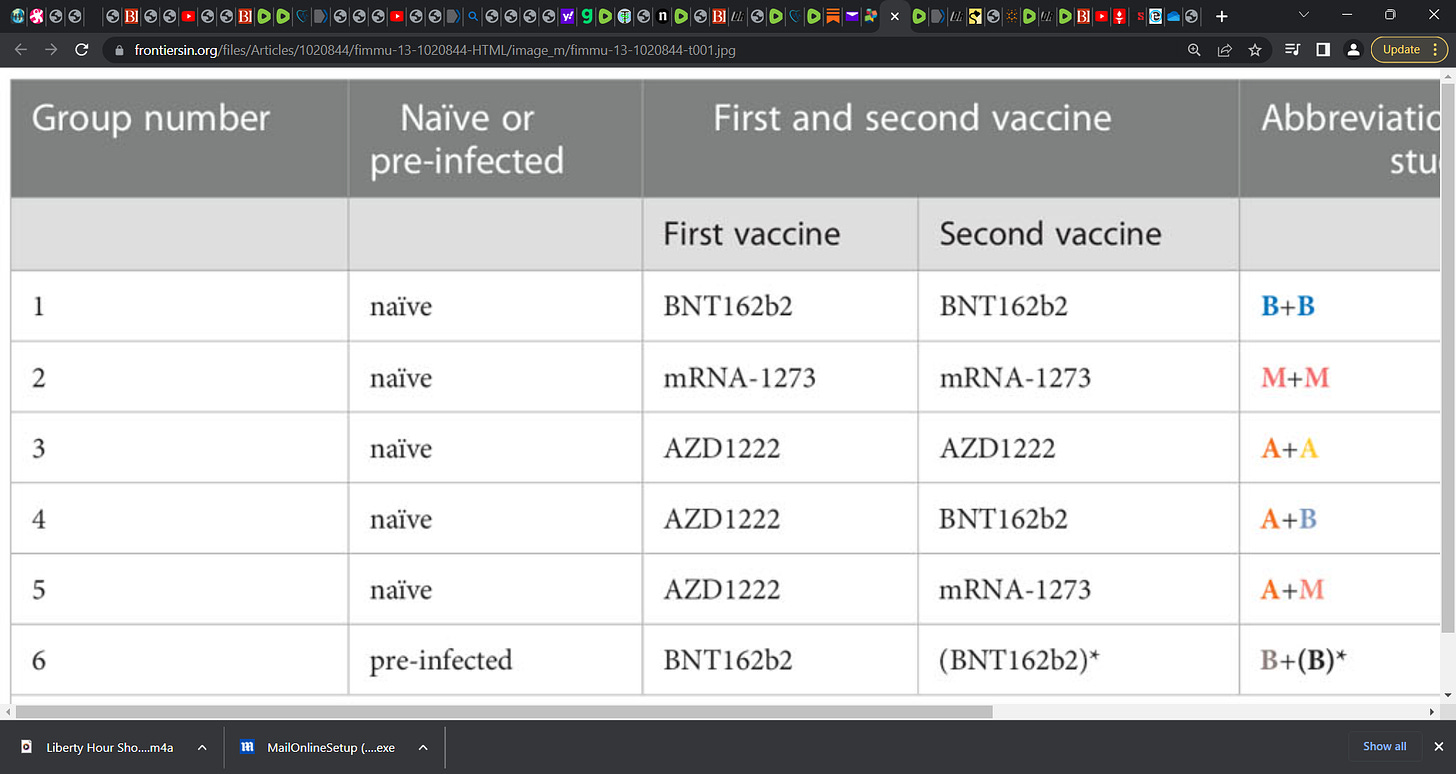
In the Buhre study above, researchers examined anti-S Ab responses in the blood and saliva of SARS-CoV-2 naïve as well as non-hospitalized persons in receipt of two doses; the researchers examined the anti-S Ab responses via receipt of different mRNA- and adenovirus-based vaccines and up to 270 days follow-up.
TABLE 1 Vaccination study groups:
Key findings:
‘Both mRNA- and adenovirus-based vaccines generate comparable long-term anti-S1 IgG1 and IgG3 levels up to day 270; whereas the IgG2 levels remained higher after mRNA vaccination. Very interestingly, two mRNA immunizations as well as one AZD1222 immunization with an mRNA booster, in particular with the mRNA-1273 vaccine, induced long-term anti-S1 IgG4 responses – the IgG subclass with inhibitory effector functions – in naïve subjects. In contrast, we could not observe such an increase upon two immunizations with the AZD1222 vaccine in naïve individuals up to day 270, suggesting that only mRNA vaccines generate detectable long-term IgG4 responses at least until day 270.’
Researchers also reported:
‘Intriguingly, the mRNA vaccines, and in particular the mRNA-1273 vaccine, induced increasing long-term anti-S1 serum IgG4 levels in naïve individuals with hitherto unclear influences on the fight against the pathogen. Naïve individuals vaccinated with the adenovirus-based vaccine did not show such long-term anti-S1 IgG4 response at least after two vaccinations until day 270.’
Note: IgG4 has a concentration of less than 5% of total IgG immunoglobulins, being the subclass with the most stable interindividual concentration. IgG4 does not activate the classical complement pathway and plays a limited role in the immune process.’ (see R Opriţă et al.).
The key Buhre et al. finding above that mirrors or supports a prior Irrgang et al. (Science Immunology) finding is that of potential immune tolerance (IgG4 switch) via class switch towards non-inflammatory, spike-specific IgG4 antibodies after repeated SARS-CoV-2 mRNA vaccination. These two papers signal potential problems with immune tolerance increasing with repeated booster doses.
Recall my prior substack on the above Irrgang’s paper and raising the question of ‘so what’? The content is relevant yet this current Buhre paper adds to the evidence and buolds the case for tolerance. What do you think?
Irrgang et al.:
Key statement:
‘We report that several months after the second vaccination, SARS-CoV-2-specific antibodies were increasingly composed of non-inflammatory IgG4, which were further boosted by a third mRNA vaccination and/or SARS-CoV-2 variant breakthrough infections. IgG4 antibodies among all spike-specific IgG antibodies rose on average from 0.04% shortly after the second vaccination to 19.27% late after the third vaccination. This induction of IgG4 antibodies was not observed after homologous or heterologous SARS-CoV-2 vaccination with adenoviral vectors.’
‘Similarly to our results (both Buhre and Irrgang), no IgG4 response was detected after two AZD1222 vaccinations. The authors observed a slight IgG4 response after immunization with AZD1222 and boosting with BNT162b2, while the effects of the mRNA-1273 vaccine were not analyzed.’
Key: Irrgang found an increase of IgG4 after the third vaccination with Pfizer.
It appears that the IgG4 class switch and tolerance is due to the mRNA and with repeated doses and principally via the Moderna gene injection.
Question is, so what? Wee Buhre et al. builds the case now for tolerance. This is a potential problem. We knew that IgG4 has the far least role in immune response that other classes have. ‘The pathophysiology of the disease is complex and should start with the description of the IgG4 molecule. IgG4 has a concentration of less than 5% of total IgG immunoglobulins, being the subclass with the most stable interindividual concentration. IgG4 does not activate the classical complement pathway and plays a limited role in the immune process.’ (see R Opriţă et al.).
Researchers also reported:
‘improved avidity and neutralizing potential of vaccine-induced antibodies after the third vaccination (9–11). However, the large number of breakthrough infections caused by the Omicron variant indicates that current vaccination regimens do not confer sterilizing protection.’










Dr. Alexander..  may I suggest that you have a scientific sub stack for those interested in the complexity of the immune system and its intricacies that  are beyond the comprehension of your non-medical reader. 
Have you seen evidence that IgE goes up with IgG4 in MultiVaxers? FLCs?