
'Permissive hypoxemia' was key strategy with our early treatment 'stay at home' NO ventilator (multidrug, sequenced) paradigm (anti-virals, corticosteroids, anticoagulants, anti-clotting drugs)
McCullough, Risch, Oskoui, Zelenko, Alexander etc. McCullough, Zelenko led the successful charge! alveoli were not clogged with fluid, but problem was blood flow to the capillaries, thus anticoagulant
Every single COVID policy failed, from lockdowns, to schools closures to the ‘not needed’ deadly COVID mRNA technology gene based injections (Bourla, Weissman, Bancel, Kariko etc. inventors), every single policy failed and only harmed and killed yet we had very early on, a treatment model that was highly effective but was denied and pilloried by governments and medical doctors when they knew it could only be effective (precautionary principle, using therapeutics with signals of benefit and that were safe, effective, cheap, available etc.):
‘This new form of hypoxemia we were observing was due to micro-blood clots in the lungs. It means the alveoli were not clogged with fluid, but the problem was blood flow to the capillaries. So by supporting the patients and providing anticoagulation, we could ride out the storm at home.’
This was our seminal paper:
The key was to keep the high-risk vulnerable person out of the death-trap hospital setting that was sure to kill or near kill grany or grandpa, our parents. Treat at home. Keep off of the ventilator.
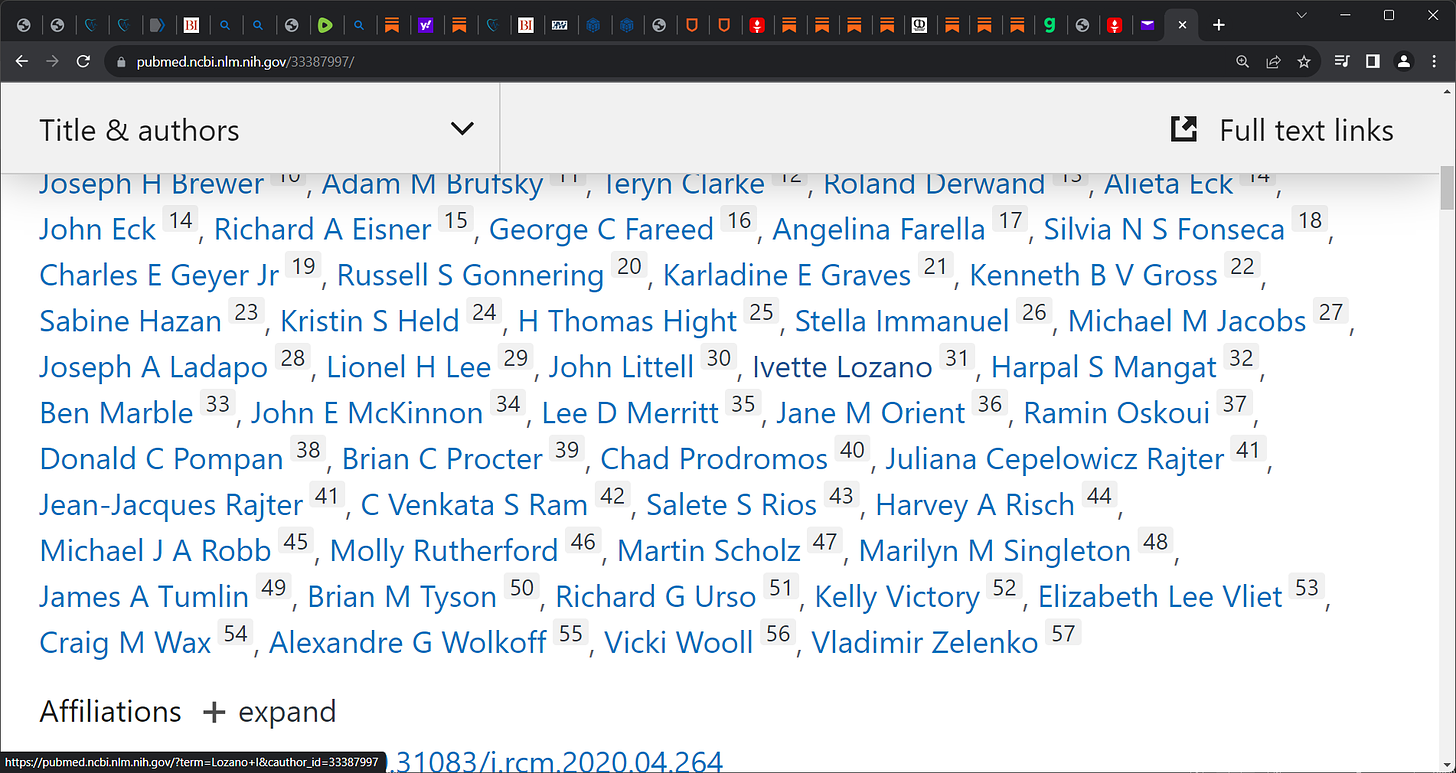
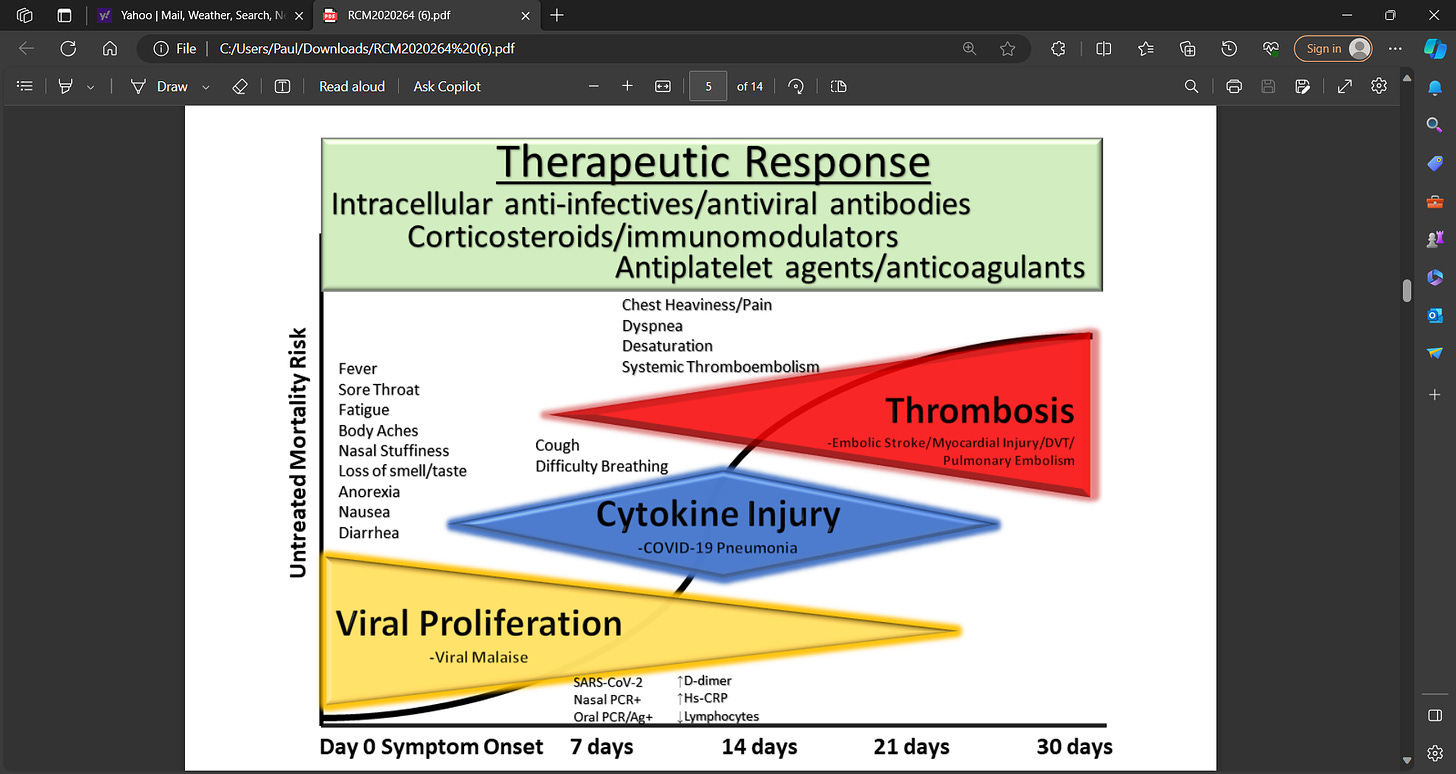
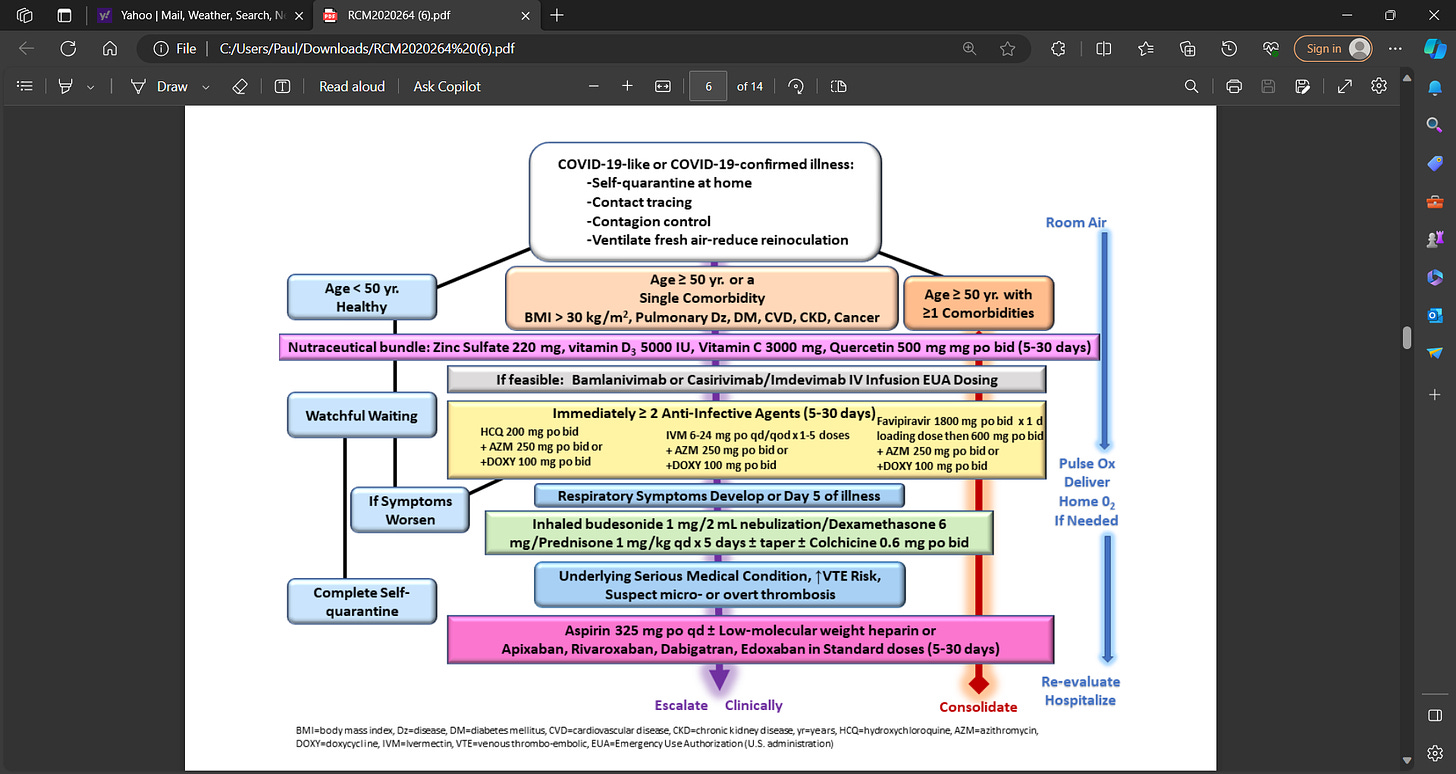
The SARS-CoV-2 virus spreading across the world has led to surges of COVID-19 illness, hospitalizations, and death. The complex and multifaceted pathophysiology of life-threatening COVID-19 illness including viral mediated organ damage, cytokine storm, and thrombosis warrants early interventions to address all components of the devastating illness. In countries where therapeutic nihilism is prevalent, patients endure escalating symptoms and without early treatment can succumb to delayed in-hospital care and death. Prompt early initiation of sequenced multidrug therapy (SMDT) is a widely and currently available solution to stem the tide of hospitalizations and death.
A multipronged therapeutic approach includes 1) adjuvant nutraceuticals, 2) combination intracellular anti-infective therapy, 3) inhaled/oral corticosteroids, 4) antiplatelet agents/anticoagulants, 5) supportive care including supplemental oxygen, monitoring, and telemedicine. Randomized trials of individual, novel oral therapies have not delivered tools for physicians to combat the pandemic in practice. No single therapeutic option thus far has been entirely effective and therefore a combination is required at this time. An urgent immediate pivot from single drug to SMDT regimens should be employed as a critical strategy to deal with the large numbers of acute COVID-19 patients with the aim of reducing the intensity and duration of symptoms and avoiding hospitalization and death.
See McCullough’s substack today with permissive hypoxemia explanation:
‘By Peter A. McCullough, MD, MPH
I have been struck with two observations throughout the COVID-19 crisis: 1) hospitalizations occurred because of lack of early ambulatory treatment, 2) nearly all the deaths occurred in hospitals, not at home.
As I was treating and advising collectively on thousands of cases over 2020 and 2021 I became very comfortable with understanding that a low oxygen saturation <94% was not a trigger for alarm. Provided the work of breathing was not too difficult and the ability to think clearly and follow instructions was solid, patients could be treated at home with supplemental oxygen then the McCullough Protocol which includes full anticoagulation. I recall treating a physician and her husband ages 58 and 60, both with severe COVID-19 pneumonia and O2 saturations in the 70’s for weeks during the Delta outbreak spanning August-September, 2021. At times saturations would dip below 70% while getting up to the kitchen or bathroom. Both of them knew they were safer at home on multidrug treatment than going to the hospital. Many hospitals had protocols that would have immediately paralyzed and sedated this couple then placed on them mechanical ventilators. This could have been the kiss of death. Yes, the couple survived with no complications and our collective confidence grew that “permissive hypoxemia” was well tolerated and very different from other forms of consolidative pneumonia, heart failure, and COPD.
This new form of hypoxemia we were observing was due to micro-blood clots in the lungs. It means the alveoli were not clogged with fluid, but the problem was blood flow to the capillaries. So by supporting the patients and providing anticoagulation, we could ride out the storm at home.
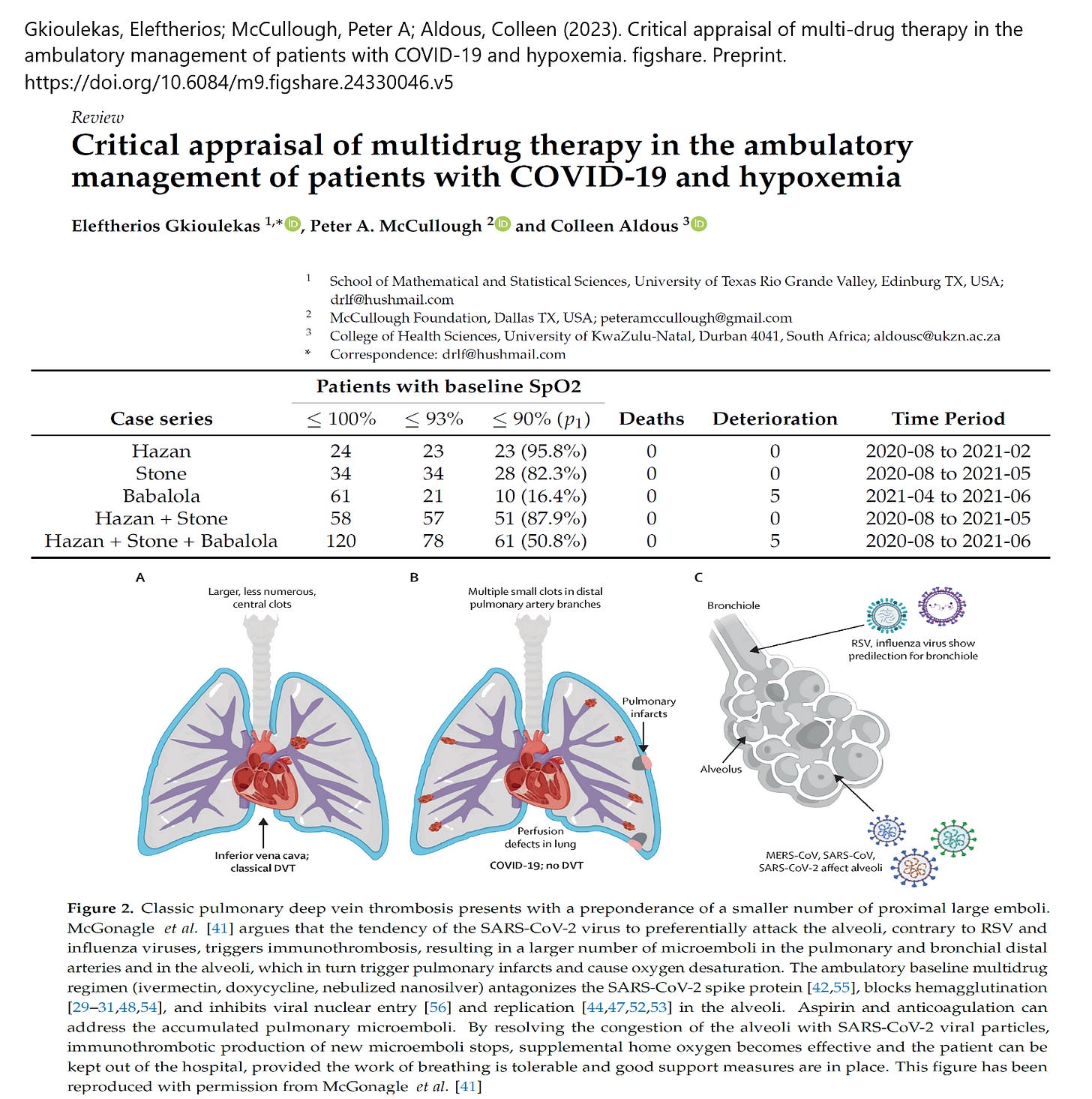
Gkioulekas et al, have published an analysis of the peer-reviewed clinical studies demonstrating safety of allowing hypoxemia to occur provided patients were treated with multidrug regimens. These papers relied heavily on the early use of ivermectin, which has an effect of unhooking the Spike protein from red blood cells, thus reducing hemagglutination and the micro-blood clotting process. The clinical results speak for themselves.
The use of the the pulse oximeter was a big mistake in the pandemic. We should have relied on clinical assessment, the work of breathing, and mentation. It’s my view that a large fraction of even the most severe cases could have been treated at home with supplemental oxygen and support. The hospitals became a death trap for COVID-19 victims as families can attest to today.’
Excellent paper by Eleftherios Gkioulekas:














Thank you Sir for your insight. I got sick Oct-Nov 2019 I’m old enough to know that this is going to be really screwed. I’m military veteran Did not will not get vaccine It’s really a shame what they did and continue to do to Our Country. Thank you for not stopping and continue to share your knowledge
Definitely highlighted the doctors and nurses willing to stand up for the patients (few) and those willing to kill them (just following orders). I'll never forget what I saw...doubt anyone will.